Key Takeaways
- Measles and German measles come from different viruses with distinct symptoms.
- Measles causes more severe illness, while German measles is milder but dangerous in pregnancy.
- Vaccination remains the best protection against both diseases.
Measles and German measles sound similar, but they come from different viruses and carry very different risks. Measles, or rubeola, spreads easily through the air and often causes high fever, cough, and a widespread rash that can lead to serious complications. German measles, or rubella, usually causes a milder illness but poses a major danger during pregnancy because it can cause birth defects. Knowing how to tell them apart helps you act quickly and protect those most at risk.
You can spot measles by its intense symptoms—high fever, red eyes, and a rash that spreads from head to toe. German measles tends to appear with a lighter rash, mild fever, and swollen lymph nodes behind the ears or neck. Both illnesses spread through respiratory droplets, making vaccination the most effective way to stop outbreaks and protect your community.
Contents
1. Overview of Measles and German Measles
- What Is Measles (Rubeola)?
- What Is German Measles (Rubella)?
- How the Viruses Differ
- Prevalence and Epidemiology
2. Key Differences in Symptoms
- Fever and Rash Patterns
- Distinctive Signs: Koplik Spots vs. Lymph Node Swelling
- Other Common Symptoms
- Symptom Duration and Onset
- Severe Complications of Measles
- Risks Associated with German Measles
- Congenital Rubella Syndrome
- Long-Term Health Impacts

Vaccination Program
Explore our range of vaccination programs designed for your specific health needs.Overview of Measles and German Measles
Both measles and German measles are viral infections that cause rash and fever, but they differ in their viral origin, severity, and long-term risks. You can better understand their impact by looking at how each virus behaves, spreads, and affects populations worldwide.

What Is Measles (Rubeola)?
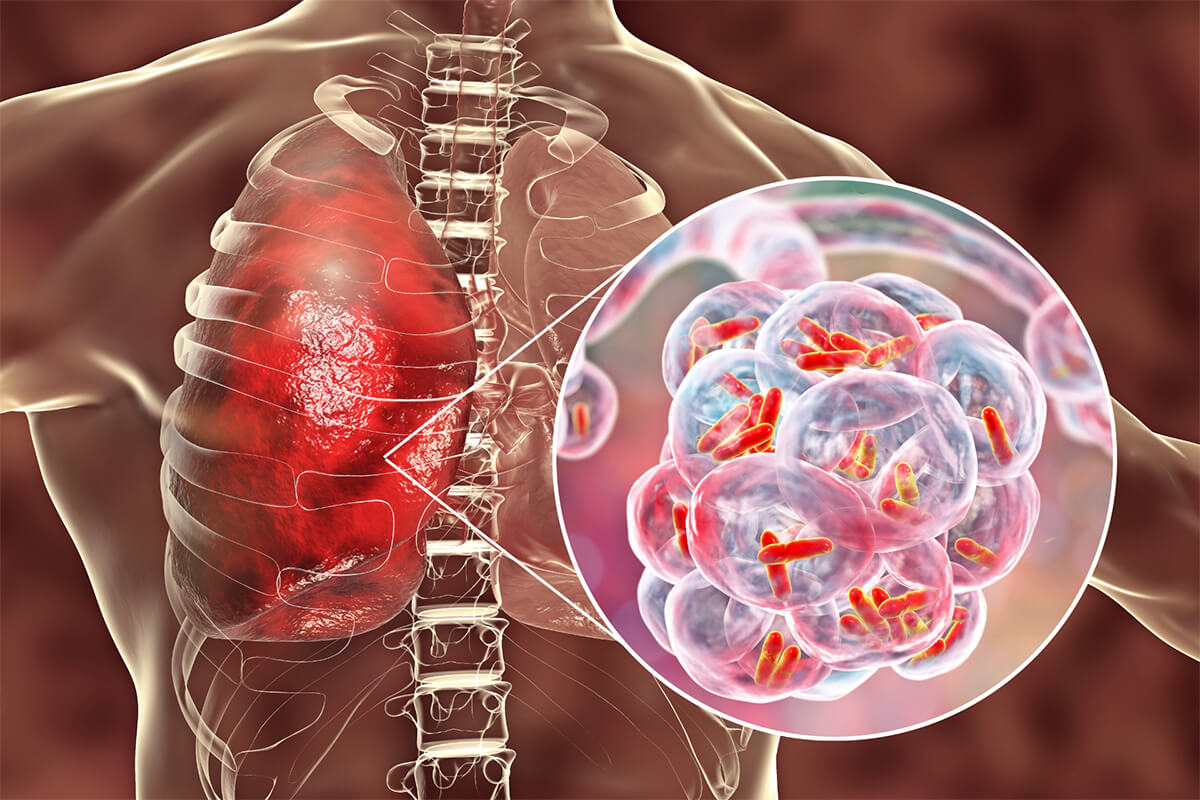
Measles, or rubeola, is a highly contagious respiratory infection caused by the measles virus, a member of the Paramyxoviridae family. It spreads through tiny droplets when an infected person coughs or sneezes.
You typically see symptoms appear 7–14 days after exposure. Early signs include high fever, cough, runny nose, and red, watery eyes. A few days later, small white Koplik spots may appear inside the mouth, followed by a red rash that spreads from the face downward.
Measles can cause serious complications, especially in young children, pregnant women, and people with weakened immune systems. Complications include pneumonia, encephalitis, and in rare cases, subacute sclerosing panencephalitis (SSPE), a fatal brain disorder that develops years after infection.
Vaccination with the MMR (measles, mumps, rubella) vaccine provides strong protection and has significantly reduced global cases, though outbreaks still occur in areas with low vaccination coverage.
What Is German Measles (Rubella)?
German measles, also known as rubella, is caused by the rubella virus from the Togaviridae family. It spreads through respiratory droplets but is less contagious and usually milder than rubeola.
You may notice low-grade fever, rash, and swollen lymph nodes, particularly behind the ears and at the back of the neck. Symptoms often last only a few days, and many people recover without complications.
However, rubella poses a major risk during pregnancy. If infection occurs in early pregnancy, it can cause congenital rubella syndrome (CRS), leading to birth defects such as deafness, heart abnormalities, or developmental delays.
Because of these severe outcomes, rubella vaccination is a key part of maternal and child health programs worldwide. The same MMR vaccine protects against both measles and rubella.
How the Viruses Differ
Although both diseases present with rash and fever, their causative viruses and clinical severity differ. The measles virus is a morbillivirus that triggers a strong immune response and often leads to high fever and extensive rash. The rubella virus is a rubivirus that typically causes milder illness.
You can distinguish them by their intensity and outcomes—measles often leads to severe complications, while rubella’s main concern is its effect on unborn babies.
Prevalence and Epidemiology
Before widespread vaccination, both measles and rubella caused large outbreaks. Global immunization campaigns have reduced their incidence dramatically, yet sporadic outbreaks still occur when vaccination rates decline.
Measles remains more common and continues to cause deaths in regions with limited healthcare access. According to global health data, it remains one of the leading causes of vaccine-preventable childhood mortality.
Rubella has been eliminated in many countries, but congenital rubella syndrome persists where vaccination coverage is incomplete. Surveillance programs monitor both viruses to prevent reintroduction and to maintain elimination status.
You help prevent these infections by ensuring full MMR vaccination coverage, which protects individuals and supports community immunity.
| Measles (Rubeola) | |
|---|---|
| Virus Family | Paramyxoviridae |
| Contagiousness | Very high |
| Rash Duration | 5-7 days |
| Major Risk | Pneumonia, encephalitis |
| Vaccine | MMR |
| German Measles (Rubella) | |
|---|---|
| Virus Family | Togaviridae |
| Contagiousness | Moderate |
| Rash Duration | 2-3 days |
| Major Risk | Congenital rubella syndrome |
| Vaccine | MMR |
Key Differences in Symptoms
Measles and German measles differ in how their fevers develop, how their rashes spread, and what distinctive signs appear during infection. You can recognize these illnesses by specific features such as rash timing, fever intensity, and the presence of either Koplik spots or swollen lymph nodes.

Fever and Rash Patterns
You will notice that measles (rubeola) causes a high fever, often reaching over 104°F (40°C), which appears several days before the rash. The rash starts on the face at the hairline and spreads downward to the trunk and limbs. The spots may merge, forming large blotches.
In contrast, German measles (rubella) produces a mild or low-grade fever, usually below 102°F (38.9°C). Its rash appears almost simultaneously with or soon after the fever begins. The rash consists of fine pink spots that start on the face and spread quickly across the body but fade within three days.
| Measles (Rubeola) | |
|---|---|
| Fever intensity | High (≥104°F) |
| Rash onset | 3–5 days after fever |
| Rash duration | 5–7 days |
| German Measles (Rubella) | |
|---|---|
| Fever intensity | Mild (<102°F) |
| Rash onset | With or soon after fever |
| Rash duration | 2–3 days |
Distinctive Signs: Koplik Spots vs. Lymph Node Swelling
In measles, Koplik spots appear inside your mouth two to three days after the first symptoms. These tiny white or bluish dots on a red background are a hallmark sign that helps confirm measles before the rash appears. They usually develop on the inner cheeks near the molars.
German measles lacks Koplik spots but often causes swollen lymph nodes, especially behind the ears, at the back of the neck, and along the base of the skull. This swelling may occur one or two days before the rash and can last for several days. The nodes may feel tender but are not usually painful.
These distinct markers—Koplik spots for measles and lymph node swelling for rubella—are key diagnostic clues that help you tell the two infections apart.
Other Common Symptoms
Both infections involve rash and fever, but the accompanying symptoms differ in severity. Measles typically causes cough, runny nose, and red, watery eyes (conjunctivitis). These symptoms appear early and often make you feel significantly ill. The cough can persist even after the rash fades.
German measles tends to cause milder respiratory symptoms or none at all. You might experience a sore throat, mild fatigue, or joint pain, especially in adults. Eye redness and cough are less common.
While measles can make you feel weak and feverish for several days, rubella often allows you to continue light activities, though you should still avoid contact with others to prevent transmission.
Symptom Duration and Onset
The timing of symptoms also helps you distinguish between the two. Measles symptoms usually begin 7–14 days after exposure, starting with fever, cough, and eye irritation before the rash develops. Once the rash appears, it lasts about a week, and recovery may take another few days.
German measles has a shorter incubation period, about 14–21 days, but its symptoms are milder and resolve faster. The rash usually lasts two to three days, and fever subsides quickly.
You may feel tired for a short time after rubella, while measles often leaves you fatigued for longer. Recognizing these differences helps you gauge the infection’s course and when to seek medical attention.
Risks and Complications
Both measles and German measles can lead to serious health problems if left unchecked. You face different levels of risk depending on your age, immune status, and vaccination history, with measles posing greater immediate danger and German measles carrying specific threats during pregnancy.
Severe Complications of Measles
Measles can cause severe illness, especially in young children, pregnant women, and people with weakened immune systems. The infection often begins with high fever, cough, and rash but may progress to life-threatening complications.
Common complications include:
- Pneumonia: the most frequent cause of death from measles in children.
- Ear infections and diarrhea: occur in up to 10% of cases.
- Encephalitis: inflammation of the brain that can cause seizures, deafness, or intellectual disability.
About 1 in 5 unvaccinated individuals who contract measles may require hospitalization. The disease spreads quickly through respiratory droplets, increasing the risk of outbreaks in unvaccinated communities.
Pregnant women infected with measles face added risks such as premature birth or low birth weight. Vaccination with the MMR vaccine remains the most effective way to prevent these complications.
Risks Associated with German Measles
German measles, or rubella, usually causes a mild illness with low fever, rash, and swollen lymph nodes. However, you should not underestimate its potential risks, especially for pregnant individuals.
While rubella rarely leads to severe illness in children or adults, it can trigger joint pain, temporary arthritis, or mild encephalitis in some cases. The infection spreads through respiratory droplets, but because symptoms can be subtle, people may unknowingly transmit the virus.
The main public health concern lies in its effect on pregnancy. Infection during early pregnancy can harm the developing fetus, making rubella vaccination essential for women of childbearing age.
Congenital Rubella Syndrome
If you contract German measles during pregnancy, particularly in the first trimester, the virus can cross the placenta and infect the fetus. This may result in Congenital Rubella Syndrome (CRS), a group of birth defects that can cause lifelong disabilities.
Possible outcomes of CRS include:
| System: Heart | |
|---|---|
| Common Effects | Congenital heart defects |
| System: Eyes | |
|---|---|
| Common Effects | Cataracts or vision loss |
| System: Ears | |
|---|---|
| Common Effects | Deafness |
| System: Nervous System | |
|---|---|
| Common Effects | Developmental delays, microcephaly |
The earlier in pregnancy infection occurs, the higher the risk of severe outcomes. Preventing rubella through vaccination before pregnancy is the most reliable protection against CRS.
Long-Term Health Impacts
Although most people recover from measles or rubella without lasting effects, some experience delayed or chronic complications. One rare but fatal condition linked to measles is subacute sclerosing panencephalitis (SSPE), which can appear years after infection and progressively damage the brain.
SSPE typically develops 7–10 years after measles infection, even if you seemed fully recovered. It causes neurological decline, seizures, and eventually loss of motor function.
German measles does not typically cause long-term illness in those who recover, but congenital rubella syndrome can result in permanent disabilities that affect hearing, vision, and cognitive development.
Vaccination not only prevents acute infection but also eliminates these long-term risks, protecting both you and future generations.
Transmission and Contagiousness
Both measles and German measles spread through respiratory droplets and close contact, but their contagiousness and outcomes differ sharply. The measles virus transmits more easily and remains infectious in the air longer, while rubella usually spreads less readily but poses serious risks during pregnancy.

How Measles Spreads
You can contract measles when you breathe in droplets or touch surfaces contaminated by the measles virus. The virus can survive in the air or on objects for up to 2 hours after an infected person leaves an area.
Even brief contact in shared spaces—such as classrooms, waiting rooms, or public transport—can lead to infection. The virus enters through the nose, mouth, or eyes and multiplies in the respiratory tract.
Because measles is highly contagious, outbreaks often occur where vaccination rates are low. One infected person can spread the virus to 90% of nearby unvaccinated individuals. Maintaining MMR vaccination coverage prevents transmission and limits community spread.
How German Measles Spreads
German measles (rubella) spreads mainly through airborne droplets released when an infected person coughs or sneezes. You can also become infected through direct contact with nasal or throat secretions.
Rubella virus transmission is less efficient than that of measles. In most cases, close and prolonged contact is required for spread. The virus does not survive long outside the body, so indirect transmission through surfaces is uncommon.
Pregnant individuals face the greatest concern. If you contract rubella during early pregnancy, the infection can cross the placenta and cause Congenital Rubella Syndrome (CRS), leading to birth defects or miscarriage. Vaccination before pregnancy remains the most effective prevention.
Contagious Periods
The measles virus becomes contagious about 4 days before the rash appears and remains so until 4 days after. You can spread the virus even before symptoms are obvious, which makes early isolation difficult.
For rubella, the contagious period starts about a week before the rash and continues for up to a week after it fades. Infants born with CRS can shed the virus for months, extending the risk of transmission.
| Infection: Measles (Rubeola) | |
|---|---|
| Contagious Before Rash | ~4 days |
| Contagious After Rash | ~4 days |
| High-Risk Transmission Source | Airborne droplets, surfaces |
| Infection: Rubella (German Measles) | |
|---|---|
| Contagious Before Rash | ~7 days |
| Contagious After Rash | ~7 days |
| High-Risk Transmission Source | Respiratory droplets, congenital infection |
At-Risk Populations
You face higher risk of infection if you are unvaccinated or immunocompromised. Children under five and adults over twenty are more likely to develop complications from measles.
For rubella, unvaccinated adults—especially women of childbearing age—are most vulnerable. Infection during pregnancy can have severe fetal consequences even if maternal symptoms are mild.
Travel to regions with ongoing outbreaks increases exposure risk. Ensuring you are up to date on measles-mumps-rubella (MMR) vaccination greatly reduces your chance of infection and helps protect those who cannot be vaccinated.
Prevention and Vaccination
You can prevent both measles and German measles through timely vaccination, high community coverage, and global monitoring of outbreaks. Immunization remains the most effective method to stop transmission and protect vulnerable groups such as infants, pregnant women, and unvaccinated adults.

MMR Vaccine Overview
The MMR vaccine protects against measles (rubeola), mumps, and rubella (German measles). It uses weakened forms of the viruses to build immunity without causing disease.
You typically receive two doses for long-term protection. The first dose is given at 12–15 months, and the second at 4–6 years. Adults without prior vaccination or evidence of immunity should also receive it, especially before travel or pregnancy planning.
The vaccine is safe and effective, with mild side effects such as low-grade fever or rash. Severe reactions are rare.
| Component: Measles (Rubeola) | |
|---|---|
| Disease Prevented | Measles |
| Type | Live attenuated |
| Typical Dose Schedule | 2 doses |
| Component: Mumps | |
|---|---|
| Disease Prevented | Mumps |
| Type | Live attenuated |
| Typical Dose Schedule | 2 doses |
| Component: Rubella (German measles) | |
|---|---|
| Disease Prevented | Rubella |
| Type | Live attenuated |
| Typical Dose Schedule | 2 doses |
Measles Vaccination Guidelines
Health authorities, including the CDC and WHO, recommend that all children receive two doses of the measles-containing vaccine. You should ensure both doses are documented to maintain immunity.
If you missed childhood vaccination, you can receive catch-up doses at any age. Pregnant women should not get the MMR vaccine until after delivery because it contains live virus components.
For international travel, you may need an early dose for infants aged 6–11 months, followed by the standard schedule later. High-risk groups such as healthcare workers and students in shared housing should confirm their vaccination status.
Keeping your immunization records updated reduces the chance of outbreaks in schools and workplaces.
Vaccination Coverage and Effectiveness
Widespread vaccination has reduced measles deaths globally by more than 70% since 2000, according to WHO data. The MMR vaccine is about 97% effective after two doses for measles and 95% effective for rubella.
However, outbreaks still occur when vaccination rates drop below 95%, the threshold needed for herd immunity. Unvaccinated individuals can spread the virus quickly, especially in crowded or international settings.
You can help maintain community protection by verifying your vaccination history and encouraging others to do the same. Public health programs rely on consistent coverage to prevent disease resurgence.
Global Prevention Efforts
Countries coordinate through the Global Measles and Rubella Strategic Plan, which aims to eliminate both diseases through vaccination campaigns and surveillance.
You may see periodic mass immunization drives targeting children under five, especially in regions with low coverage. These programs often include vitamin A supplementation to reduce complications from measles.
International organizations such as WHO, UNICEF, and GAVI support vaccine supply chains, training, and outbreak response. Their combined efforts have prevented tens of millions of deaths.
Maintaining strong public trust in vaccines and addressing misinformation remain essential to sustaining global progress.





