Key Takeaways
- Pneumonia inflames the lungs and fills the alveoli with fluid or pus.
- Recognizing symptoms early helps prevent serious complications.
- Treatment and prevention depend on identifying the cause and managing risk factors.
Pneumonia affects your lungs by causing inflammation in the tiny air sacs called alveoli, which can fill with fluid or pus and make breathing difficult. Pneumonia is a lung infection that develops when bacteria, viruses, or fungi invade the lungs and trigger inflammation that interferes with oxygen exchange. You may notice symptoms like coughing, fever, and shortness of breath that range from mild discomfort to serious illness.
You can get pneumonia anywhere—at home, work, or in a hospital setting—and anyone can be affected, though young children, older adults, and people with weakened immune systems face higher risks. Understanding what causes it and how it spreads helps you take simple steps to protect your health.
Knowing how pneumonia is diagnosed and treated gives you confidence to act quickly if symptoms appear. With proper medical care, most people recover fully, and preventive measures such as vaccination and good hygiene can reduce your chances of getting it.
Recognizing Pneumonia Symptoms
You may notice pneumonia through a combination of respiratory and whole-body symptoms. These signs often develop over several days and can vary depending on your age, health status, and the type of infection causing the illness.

Common Signs and Warning Symptoms
Pneumonia often begins with a persistent cough that may produce phlegm or pus. The cough can be dry at first and later become wet as the infection progresses. You might also experience fever and chills, which signal your body’s immune response.
Chest pain is common, especially when you breathe deeply or cough. Many people describe it as a sharp or stabbing pain. Fatigue and shortness of breath may make daily activities more difficult.
Other symptoms can include nausea, vomiting, diarrhea, and loss of appetite. In some cases, you might feel confused or disoriented, particularly if you are older. These symptoms can range from mild to severe depending on the infection’s cause and your overall health.
| Symptom Type: Respiratory | |
|---|---|
| Common Examples | Cough, chest pain, shortness of breath |
| Symptom Type: Systemic | |
|---|---|
| Common Examples | Fever, chills, fatigue |
| Symptom Type: Digestive | |
|---|---|
| Common Examples | Nausea, vomiting, diarrhea |
| Symptom Type: Neurological | |
|---|---|
| Common Examples | Confusion, dizziness |
Stages of Pneumonia and Symptom Progression
Pneumonia usually develops through several stages as the infection spreads in the lungs. In the early stage, inflammation begins in the alveoli (air sacs), leading to a mild cough and low-grade fever.
As the infection advances, the lungs may fill with fluid or pus, a process sometimes described as red hepatization. At this point, breathing becomes more difficult, and you may develop shortness of breath and chest discomfort.
In the resolution stage, your body starts clearing the infection. The cough may persist as the lungs heal and expel remaining mucus. Recovery time varies, but fatigue and mild breathlessness can last for weeks even after other symptoms improve.
Monitoring how your symptoms change helps you and your healthcare provider track recovery progress and identify complications early.
Symptoms in Different Age Groups
Infants and young children may not always show typical pneumonia symptoms. Instead of coughing, they might breathe rapidly, grunt, or appear unusually tired. Feeding problems and vomiting can also occur.
Adults often experience a productive cough, fever, and chest pain. You might notice fatigue and chills, especially if the infection is bacterial.
Older adults and people with weakened immune systems may have subtle signs. They can develop confusion, low body temperature, or a general decline in alertness rather than a high fever. Recognizing these differences is important because delayed diagnosis can increase the risk of respiratory distress and slower recovery.
When to Seek Medical Attention
You should contact a healthcare provider if you have trouble breathing, chest pain, or a fever above 102°F (39°C) that doesn’t improve with rest or fluids.
Seek immediate care if you feel confused, have bluish lips or fingertips, or experience rapid breathing. These can indicate low oxygen levels or severe infection.
Children, older adults, and people with chronic conditions such as heart or lung disease should seek help early, even for mild symptoms. Early treatment reduces the chance of complications like respiratory failure or sepsis.
If you start antibiotics or antiviral medication, follow the full course as prescribed to support full recovery and prevent recurrence.
Causes and Types of Pneumonia
Pneumonia develops when infectious organisms or irritants cause inflammation in your lungs, filling the air sacs with fluid or pus. The source of infection—bacteria, viruses, fungi, or inhaled substances—determines the type of pneumonia and how it is treated.

Bacterial Pneumonia
Bacterial pneumonia is often the most common and can range from mild to severe. It usually starts when bacteria enter your lungs after a cold or flu weakens your immune system.
The bacterium Streptococcus pneumoniae causes most community-acquired cases. Other bacteria, such as Haemophilus influenzae and Staphylococcus aureus, may also be responsible. You might experience a sudden fever, chills, chest pain, and a productive cough with green or yellow phlegm.
Doctors typically treat bacterial pneumonia with antibiotics. The specific medication depends on the bacteria involved and your overall health. People with chronic illnesses, older adults, and smokers face higher risks. Vaccines like the pneumococcal vaccine can help prevent infections caused by Streptococcus pneumoniae.
Viral Pneumonia
Viral pneumonia occurs when viruses infect your respiratory tract and spread to the lungs. Common causes include influenza (flu), respiratory syncytial virus (RSV), and SARS-CoV-2, the virus responsible for COVID-19.
Symptoms often develop gradually and may include fever, dry cough, fatigue, and shortness of breath. In many cases, viral pneumonia is less severe than bacterial forms, but it can still lead to serious complications in young children, older adults, or people with weakened immune systems.
Antibiotics do not work against viruses. Instead, treatment focuses on rest, fluids, and fever control. Antiviral medications may help in specific cases, such as influenza or COVID-19. Good hygiene, annual flu shots, and COVID-19 vaccination reduce your risk of viral pneumonia.
Fungal Pneumonia
Fungal pneumonia is less common and usually affects people with weakened immune systems or chronic lung disease. It develops when fungal spores are inhaled and settle in the lungs.
Common fungi include Histoplasma capsulatum, found in soil contaminated by bird or bat droppings; Coccidioides, which causes valley fever in dry regions; and Cryptococcus, often linked to bird droppings. Symptoms may include cough, fever, and fatigue that develop slowly over time.
Doctors diagnose fungal pneumonia using imaging and lab tests. Treatment involves antifungal medications rather than antibiotics. You are more likely to get fungal pneumonia if you take immunosuppressive drugs or have conditions such as HIV/AIDS.
Aspiration and Other Types
Aspiration pneumonia occurs when you accidentally inhale food, liquids, vomit, or saliva into your lungs. This can happen if you have swallowing difficulties, a neurological disorder, or reduced consciousness from alcohol, medication, or anesthesia.
The material inhaled introduces bacteria into your lungs, causing inflammation and infection. Symptoms may include coughing after eating, chest discomfort, and difficulty breathing.
Other forms include Mycoplasma pneumoniae infection, sometimes called “walking pneumonia,” which causes mild symptoms like a persistent dry cough and fatigue. It spreads easily in crowded places such as schools or dormitories.
Treatment for aspiration pneumonia often involves antibiotics and supportive care. Preventive steps include careful swallowing techniques, proper oral hygiene, and managing conditions that affect your ability to swallow safely.
Risk Factors and Prevention
Pneumonia risk increases when your body’s defenses are weakened or when you are exposed to harmful germs and irritants. You can lower your chances of getting pneumonia through vaccination, healthy habits, and by managing chronic health conditions effectively.

Who Is Most at Risk?
You face a higher risk of pneumonia if you are very young, over 65, or have certain long-term health conditions. Chronic illnesses such as asthma, COPD, heart disease, and diabetes can make your lungs more vulnerable to infection.
A weakened immune system also increases risk. This includes people receiving cancer treatment, those who have had an organ transplant, or those living with HIV or AIDS. These conditions reduce your body’s ability to fight off bacteria and viruses.
Older adults may also have weaker cough reflexes or less lung elasticity, which makes it harder to clear infections. Infants and young children are at risk because their immune systems are still developing.
Lifestyle and Environmental Factors
Certain behaviors and surroundings can affect your likelihood of developing pneumonia. Smoking damages the airways and reduces your lungs’ ability to clear germs, making infections more likely. Exposure to secondhand smoke or air pollution can have a similar effect.
Poor nutrition, lack of sleep, and high stress can weaken your immune system. A balanced diet rich in fruits, vegetables, and lean proteins supports immune health.
Good hygiene helps reduce exposure to infectious agents. You can lower your risk by:
- Washing your hands regularly
- Disinfecting frequently touched surfaces
- Covering coughs and sneezes
- Avoiding close contact with people who are ill
Vaccination and Preventive Measures
Vaccines play a key role in pneumonia prevention. The pneumococcal vaccine protects against common bacterial causes of pneumonia, while the flu shot helps prevent influenza-related pneumonia.
Children and some adults benefit from the Haemophilus influenzae type b (Hib) vaccine. People with chronic conditions or weakened immunity should discuss COVID-19 and RSV vaccines with their healthcare provider.
Maintaining a healthy lifestyle—staying active, eating well, and managing chronic diseases—further strengthens your body’s defenses. Quitting smoking and keeping follow-up appointments with your doctor help prevent complications and keep your lungs healthy.
Diagnosis and Medical Evaluation
When you develop symptoms that suggest pneumonia, healthcare providers use a combination of physical assessment and diagnostic tests to confirm the infection, identify its cause, and measure its impact on your lungs and oxygen levels. Accurate evaluation helps guide treatment and reduce the risk of complications.
Clinical Examination and Medical History
Your doctor begins by reviewing your medical history and asking about recent illnesses, travel, and exposure to infectious agents. They also check for underlying conditions that may increase your risk, such as chronic lung disease or a weakened immune system.
During the physical exam, your doctor uses a stethoscope to listen for abnormal lung sounds like crackles or wheezing, which can indicate fluid or infection in the air sacs. They may observe your breathing rate, heart rate, and temperature to assess how your body is responding.
You should mention any symptoms such as persistent cough, chest pain, or shortness of breath. This information helps your doctor determine whether pneumonia is likely and what further testing is needed.
Key Diagnostic Tests
A set of tests confirms the diagnosis and identifies the cause. Common options include:
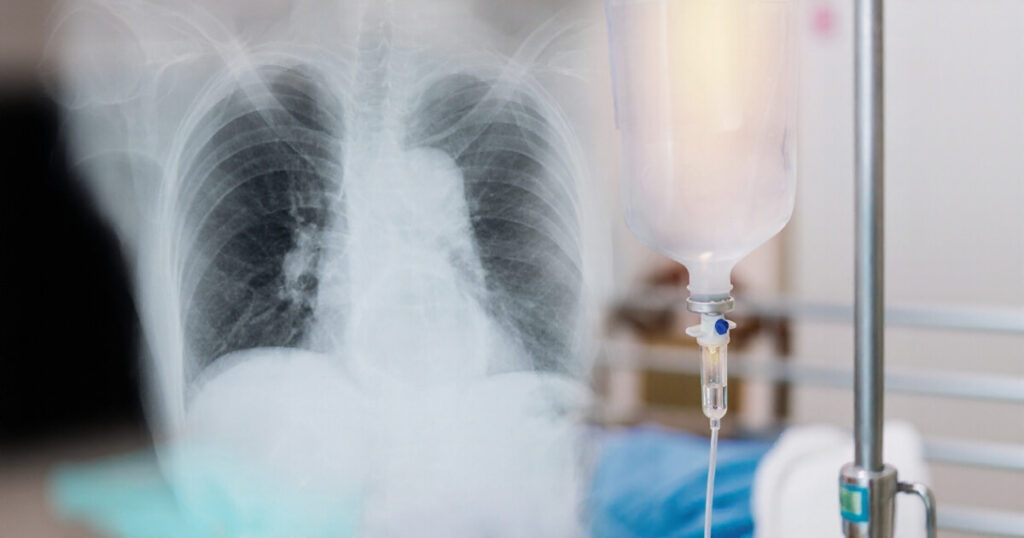
| Test: Chest X-ray | |
|---|---|
| Purpose | Shows the location and extent of lung infection |
| Test: Blood tests | |
|---|---|
| Purpose | Detect infection and sometimes identify the organism |
| Test: Sputum test | |
|---|---|
| Purpose | Examines mucus from your lungs to find bacteria or viruses |
| Test: Pulse oximetry | |
|---|---|
| Purpose | Measures blood oxygen levels to check lung function |
If your symptoms are severe or not improving, your doctor may order a CT scan for a more detailed image of your lungs. In certain cases, a bronchoscopy may be used to directly view the airways or collect fluid samples. A pleural fluid culture can identify infections in the space around the lungs.
Assessing Severity and Complications
Doctors assess how serious your pneumonia is to decide whether you need hospital care. They look at oxygen levels, blood pressure, and breathing rate to gauge how well your lungs are working.
Older adults, young children, or people with chronic conditions often need closer monitoring. Severe cases may require oxygen therapy or even mechanical ventilation.
Complications can include pleural effusion (fluid buildup), abscess formation, or sepsis. Early evaluation and prompt treatment help prevent these outcomes and support a safer recovery.
Treatment and Managing Complications
Pneumonia treatment focuses on eliminating the infection, easing symptoms, and preventing serious complications such as respiratory failure or sepsis. The approach depends on the cause of the infection, your age, and your overall health condition.

Medications and Supportive Care
Your doctor may prescribe antibiotics, antivirals, or antifungal medications depending on the germ responsible for your pneumonia. Bacterial pneumonia usually responds to antibiotics, while viral cases may require antiviral medications such as oseltamivir if influenza is involved. Fungal pneumonia is treated with antifungal drugs like fluconazole.
You may take pain relievers and fever reducers such as acetaminophen or ibuprofen to lower fever and ease discomfort. These medicines help you rest and recover more comfortably.
Supportive care plays an important role. Oxygen therapy may help if your oxygen levels are low. Breathing treatments like nebulized medications can open airways and improve airflow. Staying hydrated and taking your full course of medication reduces the risk of recurrence or drug resistance.
Hospitalization and Severe Cases
You may need hospitalization if your pneumonia is severe, your oxygen levels drop, or you have other health conditions that complicate recovery. Hospital care allows for close monitoring and rapid treatment adjustments.
In the hospital, doctors may provide intravenous (IV) antibiotics, fluids, and oxygen therapy to stabilize your breathing and circulation. If your lungs cannot supply enough oxygen, you might need a breathing machine (ventilator) for temporary support.
Older adults, infants, and people with weakened immune systems face higher risks of serious illness. In these cases, hospital care helps prevent respiratory failure, sepsis, or organ failure that can occur if pneumonia spreads or worsens.
Potential Complications and Recovery
Complications can include pleural effusion (fluid buildup around the lungs), lung abscess, or septic shock. Doctors may drain fluid from the pleural space or use imaging tests to monitor healing. Prompt treatment lowers the chance of these problems.
Recovery takes time. Fatigue and mild cough may last for weeks even after the infection clears. Rest, hydration, and gradual return to activity support healing.
To reduce future risk, keep up with vaccinations, avoid smoking, and manage chronic conditions such as diabetes or heart disease.