Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. Early diagnosis and treatment of syphilis are crucial to prevent severe complications. This comprehensive guide aims to shed light on the process of diagnosing and testing for syphilis. By understanding the various stages of the disease and recognizing its symptoms, individuals can take proactive steps towards timely testing. The article will explore different diagnostic methods, including serological tests like VDRL and RPR, direct microscopic examination, and PCR tests. Additionally, it will discuss when to get tested, preparation for testing, interpreting test results, and the importance of partner notification and contact tracing. By providing this information, we hope to encourage individuals to seek proper medical evaluation and treatment for syphilis.
Syphilis : Risk Factors and Transmission
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. It has plagued humanity for centuries, and despite advancements in medicine, syphilis remains a global health concern. To effectively combat the spread of this disease, it is crucial to understand its risk factors and modes of transmission. This comprehensive article aims to shed light on these aspects, empowering individuals to make informed decisions and take proactive measures to protect themselves.
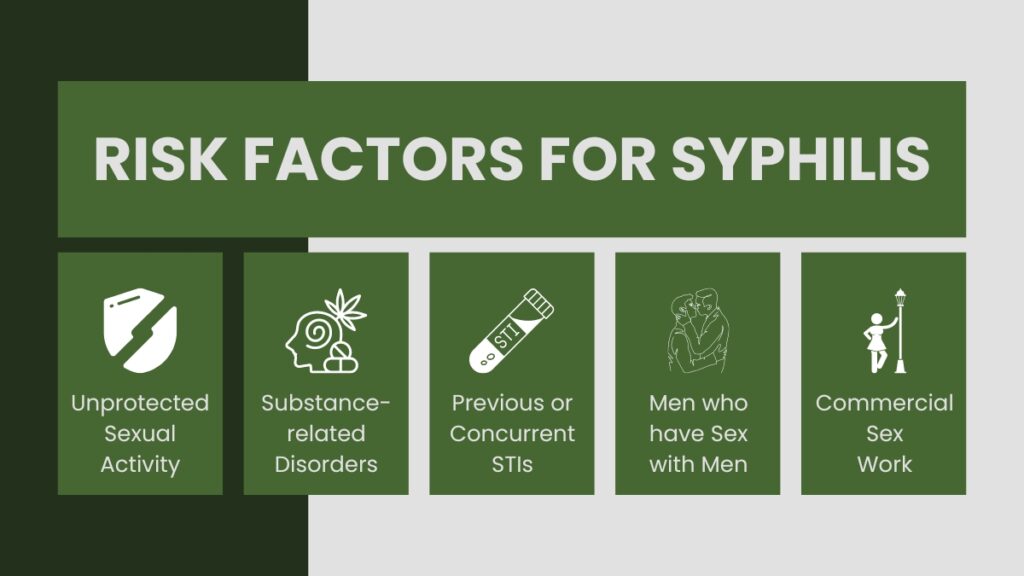
Risk Factors for Syphilis
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. It can affect individuals of any gender, age, or sexual orientation. While anyone who engages in unprotected sexual activity can be at risk, certain factors can increase the likelihood of acquiring Treponema Pallidum Disease. Understanding these risk factors is essential for prevention and early detection. Here are some significant risk factors associated with syphilis:
- Unprotected Sexual Activity: Engaging in sexual activity without using a barrier method, such as condoms, significantly increases the risk of Treponema Pallidum Disease transmission. This includes vaginal, anal, and oral sex. Having multiple sexual partners without consistent condom use raises the chances of encountering an infected individual.
- Men who have Sex with Men (MSM): Syphilis rates are disproportionately higher among MSM compared to the general population. Factors contributing to this increased risk include higher prevalence of other STIs, multiple sexual partners, and engaging in high-risk sexual behaviors such as receptive anal intercourse without a condom. Lack of access to healthcare and prevention services can further compound the risk for MSM.
- Substance Abuse: Substance abuse, particularly the use of drugs and alcohol, can impair judgment and increase the likelihood of engaging in risky sexual behaviors. Under the influence, individuals may be less likely to use protection and make informed decisions about their sexual health, thus increasing their vulnerability to Treponema Pallidum Disease and other STIs.
Syphilis-related risk elements
- Commercial Sex Work: Individuals involved in commercial sex work may face a higher risk of syphilis due to frequent changes in sexual partners, inconsistent condom use, and limited access to healthcare and prevention resources. Lack of control over the sexual encounters and the potential for violence or coercion also contribute to the risk.
- Previous or Concurrent STIs: Having a history of other STIs, such as gonorrhea or chlamydia, increases the risk of acquiring Treponema Pallidum Disease. Infections that cause genital ulcers, like herpes, also facilitate the entry of the syphilis bacteria into the body.
- Early Sexual Activity: Initiating sexual activity at a young age without proper education, access to healthcare, and awareness of safe sex practices can increase the risk of syphilis and other STIs. Young individuals may be more susceptible to engaging in risky behaviors and less likely to seek testing and treatment.
- Geographic Location: Syphilis rates can vary geographically, with certain regions or communities experiencing higher prevalence. Factors such as inadequate access to healthcare, higher rates of poverty, limited education on sexual health, and stigma surrounding STIs can contribute to the increased risk in specific areas.
It is important to note that anyone who engages in unprotected sexual activity can be at risk of Treponema Pallidum Disease. Regardless of these risk factors, practicing safe sex, getting tested regularly and seeking timely treatment are crucial for preventing the transmission and spread of syphilis.

Transmission of Syphilis
Syphilis is primarily transmitted through sexual contact with an infected individual. The bacterium Treponema pallidum, which causes syphilis, can enter the body through mucous membranes or breaks in the skin. Understanding the modes of transmission is vital for prevention and taking appropriate precautions. Here are the main ways Treponema Pallidum Disease can be transmitted:
Sexual Transmission
The most common mode of syphilis transmission is through sexual activity. This includes vaginal, anal, and oral sex with an infected person. Treponema Pallidum Disease can be transmitted even if there are no visible symptoms or if the infected individual is in the early stages of the infection. The presence of syphilis sores or rashes on the genitals, anus, or mouth significantly increases the risk of transmission.
Vertical Transmission (Mother to Child)
Pregnant women with syphilis can pass the infection to their unborn baby. This is known as vertical transmission or congenital syphilis. The bacterium can cross the placenta and infect the fetus, leading to serious complications and potentially life-threatening consequences. Syphilis can also be transmitted during childbirth if the mother has active sores or lesions.
Blood Transfusions and Organ Transplantation
While rare, syphilis can be transmitted through blood transfusions or organ transplantation from an infected donor. It highlights the importance of rigorous screening processes and testing to ensure the safety of blood and organ donations.
It’s worth noting that syphilis is not transmitted through casual contact, such as sharing utensils, hugging, or kissing. The bacterium cannot survive for long outside the human body, so transmission through objects or surfaces is highly unlikely.
Preventing the Transmission of Syphilis
- Safe Sexual Practices
- Consistently using condoms during sexual activity can significantly reduce the risk of syphilis transmission. It is important to use condoms correctly and consistently, covering the penis, vagina, or anus throughout the entire sexual encounter.
- Regular Testing and Early Detection
- Regular testing for syphilis and other STIs is crucial, especially for individuals who engage in high-risk sexual behavior or have multiple sexual partners. Early detection allows for timely treatment, reducing the risk of transmission and preventing complications.
- Partner Notification and Contact Tracing
- If diagnosed with syphilis, it is important to notify recent sexual partners, encouraging them to get tested and seek treatment if necessary. Public health agencies may conduct contact tracing to identify and notify individuals who may have been exposed to syphilis.
- Education and Awareness
- Promoting comprehensive sexual education, raising awareness about syphilis, and providing information about prevention strategies are essential for reducing transmission rates. This includes educating individuals about the importance of safe sex practices, regular testing, and seeking medical care when needed.
Syphilis and Public Health
Syphilis is not only a personal health concern but also a significant public health issue. Its impact extends beyond individuals to communities and society as a whole. Understanding the broader implications of syphilis on public health is crucial for developing effective prevention and control strategies. Here are some key aspects of syphilis and its relationship with public health:
Rising Syphilis Rates
In recent years, there has been a concerning global resurgence of syphilis. Many countries have reported increasing syphilis rates, particularly among certain populations such as men who have sex with men (MSM) and individuals involved in commercial sex work. This upward trend poses challenges for public health authorities and highlights the need for comprehensive prevention and control measures.
Social and Economic Consequences
Syphilis can have significant social and economic consequences for individuals and communities. The physical and emotional impact of syphilis, along with the potential for long-term complications if left untreated, can lead to reduced quality of life and increased healthcare costs. Syphilis-related complications can also result in lost productivity and missed work days, impacting the economy at large.
Importance of Testing and Early Detection
Timely diagnosis and treatment are vital for preventing the spread of syphilis and reducing its impact on public health. Regular testing, especially among high-risk populations, can identify cases early on and prevent further transmission. Ensuring accessible and confidential testing services is essential for encouraging individuals to seek testing and receive appropriate care.
Public Health Surveillance
Public health agencies play a crucial role in monitoring Treponema Pallidum Disease trends, collecting data, and conducting surveillance. Surveillance systems help identify areas or populations with high syphilis burden, detect outbreaks, and guide intervention strategies. By closely monitoring syphilis cases and trends, public health authorities can implement targeted prevention and control measures to mitigate the spread of the infection.
Prevention Strategies
Effective prevention strategies are central to addressing syphilis as a public health concern. These strategies include comprehensive sexual education programs, promotion of safe sex practices, widespread access to testing and treatment services, and initiatives to reduce stigma surrounding STIs. Engaging community organizations, healthcare providers, and advocacy groups is essential for implementing and sustaining effective prevention efforts.
Partner Notification and Contact Tracing
Partner notification and contact tracing are important public health measures in Treponema Pallidum Disease control. Identifying and notifying individuals who may have been exposed to syphilis helps prevent further transmission. Public health agencies work closely with healthcare providers to ensure prompt and confidential partner notification, testing, and treatment.
Research and Innovation
Ongoing research and innovation are vital for addressing the challenges posed by Treponema Pallidum Disease. This includes developing improved diagnostic tools, exploring new treatment options, and investigating strategies for effective prevention. Public health agencies collaborate with researchers, healthcare providers, and stakeholders to advance knowledge and develop evidence-based interventions.
Understanding the risk factors and transmission of syphilis is vital for promoting individual and public health. Unprotected sexual activity, multiple partners, and engaging in high-risk behaviors increase the risk of syphilis transmission. Men who have sex with men (MSM) face higher rates of infection. Treponema Pallidum Disease can be transmitted through sexual contact, vertical transmission from mother to child, and rare cases of blood transfusions or organ transplantation. Syphilis has significant social, economic, and public health consequences, necessitating regular testing, early detection, and comprehensive prevention strategies. Partner notification, contact tracing, and education are essential components of Treponema Pallidum Disease control. By prioritizing prevention, testing at Phuket Medical Clinic and treatment, we can work towards reducing the prevalence of Treponema Pallidum Disease and improving overall health outcomes for individuals and communities.
The Role of Healthcare Providers in STI Testing & Treatment
Sexually transmitted infections (STIs) are a group of infections transmitted through sexual contact, comprising bacterial, viral, and parasitic pathogens. These infections pose significant public health concerns globally, affecting individuals of all ages and genders. STIs can be asymptomatic or cause a range of symptoms, including genital ulcers, discharge, and pelvic pain. Common STIs include chlamydia, gonorrhea, syphilis, herpes, human papillomavirus (HPV), and HIV. The prevalence of STIs remains alarmingly high, with millions of new cases reported annually. Lack of awareness, stigma, and inadequate access to healthcare services contribute to the spread of these infections. Early detection, testing, and prompt treatment by healthcare providers play a crucial role in curbing STI transmission and improving overall sexual health.
Symptoms of STIs and signs of different
Sexually transmitted infections (STIs) pose a significant public health challenge worldwide, affecting millions of people each year. Early detection of STIs is of paramount importance as it plays a crucial role in preventing their spread and mitigating potential complications. Many STIs may initially present with mild or even no symptoms, making them difficult to identify without proper testing. However, untreated STIs can lead to severe health consequences, such as infertility, chronic pain, and an increased risk of HIV transmission. Furthermore, identifying STIs at an early stage allows for timely and effective treatment, reducing the risk of long-term health issues and promoting overall well-being. Educating individuals about the importance of early detection empowers them to seek timely testing and adopt preventive measures, fostering healthier and safer sexual practices.
Comprehensive Health Care at Phuket Medical Clinic
Phuket Medical Clinic (PMC) is a premier healthcare provider located in the heart of Phuket, offering an array of medical services to both local residents and international tourists. PMC combines a team of dedicated healthcare professionals, state-of-the-art facilities, and a patient-centered approach to provide top-notch medical services.
Services Offered by PMC
PMC provides comprehensive healthcare services encompassing general medicine, specialist consultations, emergency care, health check-ups, laboratory services, and more. Each service is designed to meet the diverse healthcare needs of our patients. [Expand on each service, their importance, and how PMC excels in these areas.]
Expert Healthcare Team
The backbone of PMC’s exceptional service is its team of highly qualified and experienced medical professionals. This includes doctors, nurses, and support staff who are committed to providing compassionate care to every patient. [Expand on their qualifications, experience, and commitment.]
State-of-the-art Facilities
PMC houses advanced medical equipment and facilities to ensure accurate diagnosis and effective treatment. [Expand on the different facilities, their importance, and how they contribute to excellent patient care.]
Patient-Centered Care
At PMC, we prioritize the needs of our patients. Our approach to healthcare is rooted in understanding and addressing individual healthcare needs to provide personalized care for every patient. [Expand on this philosophy, its importance, and how it is implemented at PMC.]
Easy Access for Tourists
PMC’s strategic location in Phuket makes it easily accessible for tourists seeking quality healthcare during their stay. [Expand on the services for tourists, their importance, and how PMC caters to these needs.]
PMC stands as a beacon of quality healthcare in Phuket. Our comprehensive services, expert team, state-of-the-art facilities, and patient-centered approach come together to ensure your health is in capable hands.
The importance of regular HIV testing while on PrEP
Regular HIV testing is an essential component of maintaining sexual health and preventing the spread of HIV, especially for individuals on Pre-Exposure Prophylaxis (PrEP). PrEP is a highly effective preventive medication that reduces the risk of contracting HIV. However, relying solely on PrEP without regular testing may lead to missed opportunities for early detection and timely intervention. Regular HIV testing while on PrEP serves multiple purposes: it helps identify early HIV infection, monitors the effectiveness of PrEP, and prevents the development of drug resistance. In this article, we will explore the importance of regular HIV testing for individuals on PrEP, the benefits it offers, the recommended testing frequency, and the significance of combining testing with PrEP usage. By prioritizing regular testing, individuals on PrEP can ensure their sexual health and contribute to HIV prevention efforts.
PrEP at Phuket
“Phuket Medical Clinic” is a service center for Pre-exposure prophylaxis (Prep), specializing and committed to protecting your health from HIV.
Phuket Medical Clinic: Prep service center in Phuket Preventing HIV is an important issue that everyone should pay attention to. Taking Prep medication is a highly effective way of preventing HIV and it’s a service we are committed to providing.
At “Phuket Medical Clinic”, we have a team of HIV and Prep specialists ready to provide advice and excellent care. You will receive risk assessments, annual health checks, and counseling to ensure that using Prep is the right choice for you.
HIV is a disease that can be sexually transmitted. Using Prep medication is highly effective in preventing HIV. The use of Prep is an effective method of HIV prevention that can help prevent HIV infection up to 99%.
What is Prep?
Prep, or Pre-exposure prophylaxis, is a preventive HIV medication for people at high risk of infection. Taking Prep medication can help reduce the risk of HIV infection when exposed to the virus.
How does Prep work?
Prep works by blocking the HIV virus from growing in the body. Typically, taking Prep should be combined with the use of condoms to prevent HIV and other sexually transmitted diseases.
Using Prep
Prep use should be discussed with a doctor and include an annual health check. If you are at high risk of HIV infection, such as having a partner infected with HIV or engaging in high-risk sexual behaviors, a doctor will recommend using Prep.
Side effects of Prep
Side effects of Prep are often a concern for users, but in reality, the side effects of Prep typically do not last long and disappear within two to three weeks after starting the medication.
Phuket Medical Clinic: Prep service center in Phuket At “Phuket Medical Clinic”, we have a team of HIV and Prep specialists ready to provide advice and excellent care. You will receive risk assessments, annual health checks, and counseling to ensure that using Prep is the right choice for you.
Using Prep can effectively prevent HIV infection. If you are at high risk of HIV infection, taking Prep may be the best method of prevention. If you have questions or want more information about Prep, you can contact “Phuket Medical Clinic”.
Treatment and prevention of HIV at “Phuket Medical Clinic” is not just about providing Prep. We also offer counseling, health check-ups, and continuous care. All of this is to ensure that you are confident that you are getting the best care.
เปิดบริการทุกวัน เวลา 10:00-18:00 น.
เบอร์โทร : 096-6962449
Line ID มี @ ด้วยนะครับ : @pmcphuket
แผนที่ : https://goo.gl/maps/nQ9S68sLSKwq9aoP6
What is PrEP?
PrEP (Pre-Exposure Prophylaxis) is a preventive strategy that involves the use of antiretroviral medication to reduce the risk of acquiring HIV. It is highly effective when taken as prescribed, offering protection to individuals at high risk of infection, such as those in serodiscordant relationships or engaging in unprotected sex with multiple partners. PrEP works by inhibiting the replication of HIV in the body, thereby preventing the virus from establishing an infection. This revolutionary approach has shown significant success in preventing new HIV cases and has become an essential tool in the global fight against HIV/AIDS, alongside other prevention methods.
PEP After Condom Breakage or Unprotected Sex at Phuket Medical Clinic
Taking immediate action after potential exposure to HIV is crucial to prevent the virus from taking hold in your body. Post-Exposure Prophylaxis, or PEP, can be your lifeline if you’ve had unprotected sex or experienced a condom break. In Phuket, Thailand, the Phuket Medical Clinic offers prompt and confidential PEP treatment services.
Medical Certificate at Phuket Medical Clinic
Whether you need it for travel, employment, or any other purpose, a medical certificate is a crucial document that validates your health status. In Phuket, Thailand, the trusted and reliable provider of comprehensive medical certification services is the Phuket Medical Clinic.