Skin diseases affect millions of people worldwide, causing discomfort, distress, and sometimes even serious health complications. Proper knowledge about these conditions is crucial for prevention, early diagnosis, and effective treatment. In this SEO article, we will explore some common skin diseases, their causes, symptoms, and available treatments to help you better understand and manage these conditions.
Defeating Seasonal Allergies : Guide to Relief and Prevention
Seasonal allergies, also known as hay fever or allergic rhinitis, affect millions of people worldwide. These allergies occur when the immune system overreacts to pollen, mold spores, and other environmental allergens. While they may not be life-threatening, seasonal allergies can significantly impact your quality of life during certain times of the year. This article aims to provide valuable insights into understanding, managing, and preventing seasonal allergies.
Understanding the Flu: Symptoms, Prevention, and Treatment
The flu, short for influenza, is a common viral infection that affects millions of people worldwide each year. While it may seem like a routine illness, the flu can lead to serious health complications, especially in vulnerable populations. In this SEO article, we will explore everything you need to know about the flu, including its symptoms, prevention strategies, and treatment options.
The Essential Guide to General Health Care: Tips for a Happier, Healthier You.
General health care is the cornerstone of overall well-being. It encompasses a wide range of practices, habits, and medical services that collectively contribute to a healthy and fulfilling life. In this article, we will explore the key aspects of general health care, offering valuable insights and tips to help you prioritize your health and live your best life.
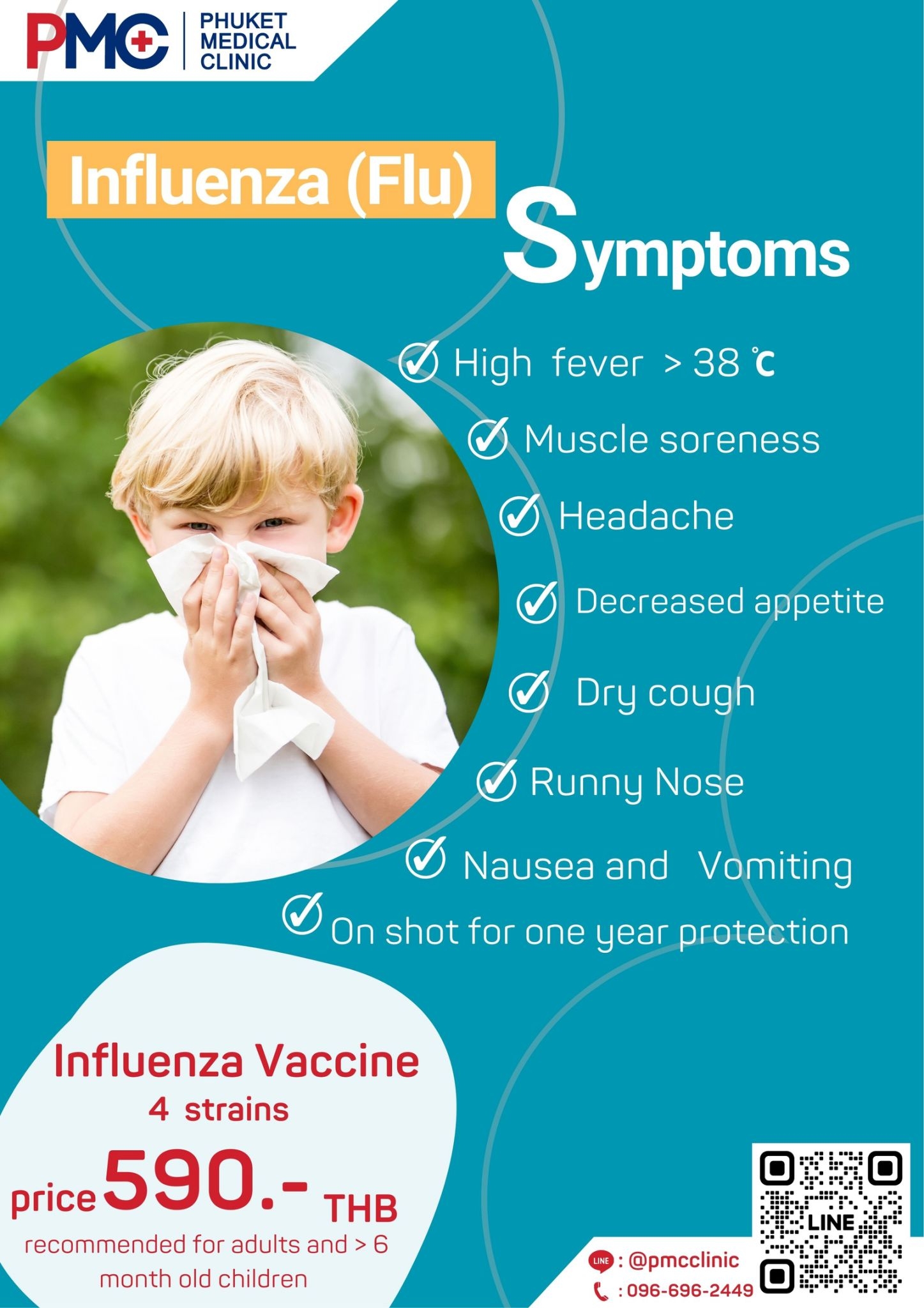
Influenza (Flu) Vaccine in Phuket
Influenza, commonly known as the flu, is caused by the influenza virus. This virus is present in the mucus, saliva, or respiratory secretions of infected individuals and is transmitted through coughing, sneezing, or breathing the same air. Once the virus infects the upper respiratory tract, it leads to symptoms such as high fever, cough, sore throat, runny nose, nasal congestion, sneezing, headache, body aches, and fatigue, similar to a common cold.
However, the symptoms can be more severe in young children under the age of 2, the elderly, and individuals with underlying chronic conditions. Complications such as pneumonia and encephalitis can arise, and the virus can exacerbate pre-existing conditions like heart disease, diabetes, liver and kidney problems, potentially requiring hospitalization. Even after recovery, the body may experience lingering fatigue for several weeks.
Therefore, preventing influenza by getting vaccinated is crucial. Vaccination plays a significant role in minimizing the risk of contracting the flu.
Influenza can be divided into 4 strains as follows:
- The Influenza virus strain A/H1N1, commonly known as the Novel Influenza A (H1N1) or the 2009 H1N1 pandemic flu, is a contagious disease that originated in Mexico and quickly spread to various countries. This disease resulted from the reassortment of both human and animal strains of the virus, leading to a new strain that rapidly spread from person to person. Symptoms indicating this illness include high fever, runny nose, cough, and abnormal respiratory symptoms. Some individuals might also experience accompanying gastrointestinal symptoms. This disease can be treated with the antiviral medication called “Oseltamivir.”
- The Influenza virus strain A/H3N2 can be transmitted from pigs to humans and has caused severe outbreaks, particularly in Hong Kong. This strain is also referred to as the Hong Kong flu. Symptoms resembling typical flu symptoms occur, but additional symptoms may include muscle aches, rapid breathing, fatigue, and wheezing.
- The Influenza virus strain B Colorado lineage Victoria typically spreads in cold and dry weather or during the winter season. It primarily spreads from person to person. Individuals with underlying health conditions are at a higher risk of contracting this strain.
- The Influenza virus strain B Phuket lineage Yamagata is prevalent from December to January. The groups most susceptible to this strain are children under 2 years old, pregnant women, and the elderly.
The vaccine for preventing influenza, also known as the flu, is what?
The Influenza Vaccine is a type of injectable vaccine produced from inactivated virus. It undergoes a manufacturing process that ensures safety and high efficacy. While it helps prevent influenza, individuals who have received the vaccine might still experience the flu, but the symptoms tend to be milder. The influenza vaccine does not provide protection against common colds caused by other viruses.
The influenza vaccine used in Thailand is an inactivated vaccine, which comes in two groups:
- The group that consists of the major strains of the Influenza virus for the trivalent inactivated influenza vaccine are Influenza A, Influenza B, and Influenza C. However, in vigilant monitoring, only types A and B are considered seriously due to the fact that type C is less common, causes milder symptoms, and does not lead to widespread outbreaks to the extent of the first two types.
- The group that includes the major strains of the Influenza virus for the quadrivalent inactivated influenza vaccine covers four main strains of the virus, as follows:
- Influenza virus strain A/H1N1
- Influenza virus strain A/H3N2
- Influenza virus strain B lineage Victoria
- Influenza virus strain B lineage Yamagata
The World Health Organization recommends receiving the quadrivalent influenza vaccine as it is effective in providing increased coverage against influenza compared to before.
Why is it necessary to receive the influenza vaccine every year?
Getting the influenza vaccine annually is recommended because after receiving the vaccine for a certain period, the body’s immunity to the disease gradually decreases. Additionally, the strains of the influenza virus change each year. Therefore, it is necessary to get vaccinated every year to ensure that the body maintains immunity and can effectively protect against the strains currently in circulation.
- It is recommended to receive the influenza vaccine before the peak seasons of outbreaks (rainy and cold seasons). Therefore, it’s advisable to get vaccinated about 2 months in advance. This timing allows the vaccine to build a highly effective immunity in the body, which coincides with the period of potential outbreaks. Consistently getting vaccinated every year during this time is particularly crucial, especially for individuals in high-risk groups. This is because the body’s immune response to the influenza virus can decrease relatively quickly.
- Getting vaccinated every year is a way to stimulate the immune system to remain at a high level. This enables the body to maintain immunity against new strains of the influenza virus that emerge each year.
- The quadrivalent vaccine is recommended for individuals ranging from 6 months of age to adults, including the elderly, pregnant women, and breastfeeding mothers. They are all eligible to receive the influenza vaccine.
Who are the individuals recommended to receive the influenza vaccine?
- General individuals of all ages can receive the vaccine.
- Patients with chronic diseases including diabetes, cerebrovascular disease, kidney disease, asthma, chronic obstructive pulmonary disease (COPD), chronic lung disease, heart disease, liver disease, blood disorders, and those undergoing chemotherapy for cancer.
- Pregnant women at or after the 4th month of pregnancy.
- Individuals aged 65 and above.
- Children aged 6 months to 2 years.
- Individuals with severe brain injury who cannot care for themselves.
- Thalassemia patients.
- Individuals with weakened immune systems and those with symptomatic HIV infection.
- Individuals with a weight of 100 kilograms or a BMI of 35 Kg/m2.
- Individuals planning to travel abroad, especially to Europe and the Americas.
- Individuals likely to be in crowded or densely populated areas, such as those attending religious ceremonies, sports events, or various festivals.
- Medical personnel and staff involved in patient care.
Who are the individuals who should not receive the influenza vaccine?
- Children under 6 months of age.
- Individuals with muscle weakness disorders.
- Individuals who previously received the influenza vaccine and experienced severe allergic reactions to the vaccine components in a previous dose.
- Individuals with a history of severe egg allergy or allergies to various vaccine components (the influenza vaccine does not contain antibiotics and preservatives).
- If you have a sudden fever, illness, or uncontrolled chronic conditions, it’s advisable to postpone the vaccination. In the case of a minor cold without fever, the vaccine can still be administered.
Side effects of the influenza vaccine.
- Specific symptoms at the injection site, such as pain, swelling, and redness, may occur within 24-48 hours after vaccination. However, these symptoms usually resolve on their own within 2-7 days. Cold compresses can also be applied to the injection site. If any abnormal symptoms occur beyond this, it’s advisable to consult a doctor.
- After vaccination, some individuals might experience mild fever, discomfort, muscle aches, and headache. These symptoms might start within 6-12 hours and can last 1-2 days without requiring treatment.
- Severe allergic reactions are extremely rare and would typically manifest within 2-3 minutes to 2-3 hours after vaccination. Symptoms might include difficulty breathing, wheezing, hoarseness, hives, weakness, rapid heartbeat, or dizziness. If any of these symptoms occur, immediate medical attention is necessary.
What are the benefits of the quadrivalent influenza vaccine?
In addition to providing protection against the four mentioned strains of the influenza virus, the influenza vaccine offers additional benefits, including:
- The influenza vaccine can provide increased coverage against the Type B strain of the influenza virus, as the flu virus undergoes strain changes every year.
- It stimulates and strengthens the immune system.
- It reduces the rate of influenza outbreaks.
- It decreases middle ear infections in children.
- It lowers the risk of complications resulting from influenza infections, especially in young children and chronic patients.
- It reduces the need for antibiotics for secondary bacterial infections associated with influenza.
- It cuts down on healthcare expenses for treatment.
- It minimizes work or school absenteeism.
- It decreases hospitalization costs.
- It reduces the mortality rate due to influenza.
- It protects patients with chronic conditions from infection risks.
- It offers influenza protection for individuals aged 65 and above, with an effectiveness rate of 60%.
Where can you receive the influenza vaccine in Phuket?
Phuket Medical Clinic : Close, Expert Care. Dedicated Medical Professionals and Skilled Team providing Consultation and Treatment. Walk-in or Scheduled Appointments for Convenient and Efficient Services.
Book an appointment online : https://phuketmedicalclinic.youcanbook.me
Daily Open 🕙 10:00-18:00
Contact number ☎️ 096-696-2449
Line id : @pmcphuket or https://lin.ee/R1TKRDo
Map 📌https://goo.gl/maps/xu45eTQUTjgpukJa7
Website 🌐https://phuketmedicalclinic.com
Feel free to consult with a doctor or ask further questions anytime.
Inbox : m.me/100483916443107
#healthcareclinic #คลินิกภูเก็ต
Phuket #Clinic #ภูเก็ตเมดิคอลคลินิก
#Phuketmedicalclinic
Vaccinenation Services in Phuket
Vaccinenation, or the process of getting vaccinated, is a crucial part of any healthcare system. It not only prevents the spread of infectious diseases but also ensures the overall well-being of the community. With the influx of tourists and the potential for diseases to spread quickly, Phuket understands the significance of an efficient vaccinenation program.
Office Syndrome (Myofascial pain syndrome) – Phuket Medical Clinic
The current trendy disease among working-age individuals is undoubtedly “office syndrome,” which is increasingly prevalent day by day. This is due to the work behaviors of office workers, which vary from person to person. Some individuals may engage in risky behaviors, such as sitting hunched over, spending prolonged periods in front of computer screens without ergonomic adjustments, or working in an unsuitable work environment, such as desks and chairs that are too high. These factors can lead to physical discomfort and pain, and what we do in our daily lives can negatively impact our bodies, potentially causing a condition known as “office syndrome.”

What is Office Syndrome?
Office Syndrome, refers to a group of symptoms related to myofascial pain and discomfort. This condition, Myofascial Pain Syndrome, often occurs due to repetitive use of certain muscles over an extended and continuous period of time. The result of this can lead to muscle inflammation and persistent pain that radiates to other body parts. These symptoms can manifest from the neck, back, waist, shoulders, arms, and even extend to the wrists. If individuals experience Office Syndrome symptoms but do not seek immediate treatment upon its onset, the condition can worsen and the pain can spread, leading to chronic discomfort.
What causes Office Syndrome
Most of the muscle pain symptoms associated with Office Syndrome are commonly found in individuals who primarily work in office settings. This is due to work habits that involve prolonged and focused computer screen usage, often leading to neglect of bodily movements and changes in posture. Typically, there’s minimal physical activity or transitions, which results in various muscle groups becoming tense, contracted, and inflamed.
Symptoms of Office Syndrome
- Specific Muscle Pain : Occurrence of localized muscle pain, often with a generalized and unclear distribution. This pain is commonly felt around the neck, shoulders, back, hips, and lower back. It tends to be chronic and persistent.
- Chronic Headaches : Persistent headaches or migraines that stem from prolonged stress and prolonged use of the eyes focused on computer screens over an extended period.
- Back Pain : Back pain is a common symptom among Office Syndrome patients due to prolonged hours of continuous computer screen usage. Additionally, poor sitting posture contributes to the constant strain on the muscles, leading to consistent fatigue and stiffness. This is especially evident in those who habitually hunch their backs, including women who wear high heels while standing for extended periods in an office environment.
- Leg Pain and Numbness : Leg pain and numbness can arise from sitting in the same position for extended periods, leading to compression of blood vessels and disrupted blood circulation.
- Eye Strain : Blurry vision, eye fatigue, and discomfort resulting from prolonged and intense visual concentration on computer screens.
- Hand Tingling and Pain : Numbness and a locked feeling in fingers and hands caused by extended use of computer mice without variation in hand movements. This constant pressure on nerves can lead to inflammation and pain.
- Muscle Inflammation : Swelling or tenderness in muscles, often occurring in the shoulders, elbows, ankles, knees, and wrists. Such inflammation can result from accidents, vigorous activities, or excessive and repetitive use, leading to localized pain and discomfort.

Treatment of Office Syndrome
There are many methods, including treating office syndrome with medicine. working environment adjustment physical therapy to stretch Exercise to treat back pain and increase physical fitness. and adjust the car’s posture to be correct Treatment with alternative sciences such as acupuncture, Thai massage, etc.
Initially, the treatment will focus on physical therapy. Behavior modification, which is the solution to the root cause of office syndrome. And can cause the injury of the body in that part to be reduced.
- Reduce muscle pain caused by muscle tension and inflammation. Avoid using or limiting movement of the affected joints such as shoulders, wrists, and elbows. Physical therapy or using assistive devices may be necessary in some cases.
- Stretching the muscles properly is essential as it helps lengthen tendons and muscle fibers, improving joint flexibility and range of motion. This can prevent muscle fiber tears and reduce the risk of injuries.
- Minimize risk factors that contribute to pain. Avoid prolonged repetitive tasks in the same posture, incorrect work postures, and ensure that frequently used items are within easy reach without needing to bend or stretch excessively. Manage work and rest schedules appropriately.
- Adjust your working posture according to ergonomic principles by adjusting the equipment you use, including the desk, chair, workspace lighting, computer screen, and other tools, to make them suitable for your body.
- Traditional Thai massage is the primary method of pain relief that humans have known since ancient times. It’s a natural technique that stems from experiential learning, such as pressing and kneading directly on the painful areas.
- Acupuncture, utilizing mechanisms to suppress pain, helps release neurotransmitters to affect the central nervous system at the spinal cord level. This assists in pain relief, relaxes muscular trigger points, and balances various organs to a normal state.
- Taking medication is a personal matter for everyone. Therefore, before taking any medication, it’s essential to carefully read the label every time and strictly follow the instructions to ensure the medication’s efficacy.
- Engaging in physical exercise is crucial for office syndrome treatment. If your muscles are not flexible and strong enough, they won’t be able to withstand continuous use over extended periods. This could lead to recurring office syndrome that doesn’t go away.
- In this condition, exercise is crucial and can be divided into two main types, namely:
- Exercise for stretching and elongating muscles aims to enhance flexibility and reduce muscle tension often caused by prolonged repetitive activities. This stretching can be started even while experiencing pain.
- Exercise for strengthening muscles is intended to build endurance and strength in specific muscle groups. This allows these muscles to perform continuous tasks for longer periods. Such strength-building exercises are typically initiated when acute pain subsides. They often begin with isometric strengthening exercises, as these tend not to exacerbate acute pain. Subsequently, other forms of strength-building exercises can be gradually introduced in sequence.
Prevention of Office Syndrome
Preventing pain from work-related activities and achieving positive results on your own can be done through the following methods:
- Adapting the work environment to be ergonomic.
- Exercising to strengthen muscles should focus on movements involving various body parts, particularly muscles and tendons that are prone to pain.
- Stretching muscles to relieve tension in muscles used during work.
- Take breaks every hour while sitting to stand, walk around, or change positions to allow your body to rest within itself. Alternatively, find time to take a relaxing walk and give your muscles and eyes a break every hour for the best results.
- Perform light exercises using nearby objects, like using a water bottle on your work desk or squeezing a stress ball to exercise your hands.
- Using supportive equipment for prevention should not be purchased and used without consulting a doctor.
- If you find that muscle pain persists despite stretching, adjusting your work posture, or providing self-care, consult a specialized physician immediately regarding your office syndrome symptoms.
Where can you receive the influenza vaccine in Phuket?
Phuket Medical Clinic : Close, Expert Care. Dedicated Medical Professionals and Skilled Team providing Consultation and Treatment. Walk-in or Scheduled Appointments for Convenient and Efficient Services.
Book an appointment online : https://phuketmedicalclinic.youcanbook.me
Daily Open 🕙 10:00-18:00
Contact number ☎️ 096-696-2449
Line id : @pmcphuket or https://lin.ee/R1TKRDo
Map 📌https://goo.gl/maps/xu45eTQUTjgpukJa7
Website 🌐https://phuketmedicalclinic.com
Feel free to consult with a doctor or ask further questions anytime.
Inbox : m.me/100483916443107
#healthcareclinic #คลินิกภูเก็ต
Phuket #Clinic #ภูเก็ตเมดิคอลคลินิก
#Phuketmedicalclinic
Dengue Fever in Phuket: What You Need to Know and Testing
Dengue fever is a mosquito-borne viral infection that causes severe flu-like symptoms, including high fever, severe headaches, pain behind the eyes, joint and muscle pain, rash, and mild bleeding (like nose bleed or gum bleed). In rare cases, it can develop into severe dengue, which can be fatal.
Chlamydia Outbreaks: Causes and Control Measures
Chlamydia is a common sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis. It is one of the most prevalent STIs globally, affecting millions of people each year. Chlamydia is primarily transmitted through unprotected sexual activity, including vaginal, anal, or oral sex. What makes this sexually transmitted disease particularly concerning is its asymptomatic nature, as many infected individuals may not experience any noticeable symptoms. However, even without symptoms, Chlamydia can still cause severe health complications if left untreated, such as pelvic inflammatory disease (PID), infertility, and increased susceptibility to other STIs. Understanding the causes and control measures for Chlamydia outbreaks is crucial to prevent its spread, protect individual health, and promote overall sexual well-being.
Understanding Chlamydia Outbreaks
Chlamydia is a common sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis. It can infect both men and women and is typically transmitted through vaginal, anal, or oral sex with an infected individual. This sexually transmitted disease can also be passed from an infected mother to her baby during childbirth.
When it comes to understanding chlamydia outbreaks, several factors need to be considered:
- Risk factors: Certain behaviors and demographics can increase the risk of chlamydia outbreaks. Factors such as unprotected sex, multiple sexual partners, young age (15-24 years), and engaging in high-risk sexual behaviors can contribute to the spread of the infection.
- Asymptomatic nature: This sexually transmitted disease is often referred to as a “silent” infection because it frequently does not cause noticeable symptoms, especially in women. This means that infected individuals may unknowingly transmit the infection to others, leading to an increased risk of outbreaks.
- Screening and testing: Routine screening and testing for chlamydia can help identify infected individuals who may not show symptoms. Widespread screening programs, especially among high-risk populations, can play a crucial role in detecting and treating chlamydia infections, thereby reducing the likelihood of outbreaks.
- Treatment and partner notification: Prompt treatment of chlamydia infections is essential in preventing complications and further transmission. Infected individuals should receive antibiotics to clear the infection. Additionally, notifying and treating sexual partners of infected individuals is vital to prevent reinfection and break the cycle of transmission.
- Public health interventions: Public health organizations and healthcare providers play a vital role in raising awareness about chlamydia, promoting safe sexual practices, and providing accessible testing and treatment services. Educational campaigns, community outreach, and the availability of free or low-cost healthcare services can help control chlamydia outbreaks.

Causes of Chlamydia Outbreaks
Chlamydia outbreaks can be caused by a combination of factors related to the bacterium itself, individual behavior, and societal factors. Here are some key causes that contribute to chlamydia outbreaks:
Sexual Behavior
Chlamydia is primarily transmitted through sexual contact, so behaviors that increase the risk of exposure to infected individuals can lead to outbreaks. These behaviors include having unprotected sex (without using condoms or dental dams), having multiple sexual partners, and engaging in high-risk sexual activities.
Lack of Awareness and Chlamydia Education
Limited knowledge about chlamydia, its symptoms, and modes of transmission can contribute to the spread of the infection. When individuals are not aware of the risks or do not have access to accurate information, they may engage in behaviors that increase their vulnerability to chlamydia and contribute to outbreaks.
Asymptomatic Infections
Chlamydia is often asymptomatic, especially in women. Infected individuals who do not experience noticeable symptoms are less likely to seek testing and treatment, leading to ongoing transmission. As a result, outbreaks can occur as the infection spreads unknowingly.
Inadequate Screening and Testing
Limited access to routine screening and testing services for chlamydia can hinder early detection and treatment. Without regular screening programs in place, infected individuals may go undiagnosed, allowing the infection to spread further and contribute to outbreaks.
Delayed or Inadequate Treatment
Timely treatment with antibiotics is essential to control chlamydia infections and prevent their transmission. However, delayed or inadequate treatment can result from various factors, such as limited healthcare access, lack of awareness about available treatment options, or failure to complete the prescribed course of antibiotics. These factors can contribute to the persistence of chlamydia infections and facilitate outbreaks.
Population Dynamics
Certain populations, such as adolescents and young adults, have higher rates of chlamydia infection. Factors such as increased sexual activity, higher rates of partner change, and lower utilization of preventive measures can make these populations more vulnerable to outbreaks.
Socioeconomic Factors
Socioeconomic factors, including poverty, limited access to healthcare, and lack of health insurance, can impact the incidence and spread of chlamydia. Individuals facing socioeconomic challenges may have limited resources to seek healthcare services, including testing and treatment for chlamydia, which can contribute to the persistence of infections and outbreaks.

Symptoms of Chlamydia
Chlamydia is known as a “silent” infection because it often doesn’t cause noticeable symptoms, especially in women. However, when symptoms do occur, they typically manifest within one to three weeks after exposure to the infection. It’s important to note that even in the absence of symptoms, chlamydia can still cause complications if left untreated. Here are some common symptoms of chlamydia:
- Men:
- Penile discharge, a cloudy or clear discharge may be present from the tip of the penis.
- Painful or burning sensation during urination.
- Testicular pain or swelling (less common).
- Women:
- Abnormal vaginal discharge, an unusual discharge that may have a strong odor or appear watery, milky or yellowish.
- Painful or burning sensation during urination.
- Lower abdominal pain or pelvic pain.
- Painful sexual intercourse.
- Bleeding between periods or after sexual intercourse (less common).
It’s worth noting that the majority of women with chlamydia do not experience any symptoms. If left untreated, chlamydia can lead to serious complications such as pelvic inflammatory disease (PID), which can cause chronic pelvic pain, infertility, or an increased risk of ectopic pregnancy.
- Men and Women:
- Rectal Symptoms: Chlamydia can infect the rectum in individuals who engage in receptive anal intercourse. This can cause rectal pain, discharge, or bleeding.
- Throat Symptoms: Chlamydia can also infect the throat through oral sex, although throat infections are typically asymptomatic.
Prevention and Control Measures
Chlamydia is a common sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis. To prevent and control the spread of this sexually transmitted disease, a combination of public health measures and individual actions are essential. Here are some key prevention and control measures:
- Safe Sex Practices: Practicing safe sex is crucial in preventing this sexually transmitted disease transmission. This includes using condoms or dental dams correctly and consistently during sexual intercourse, especially with new or multiple partners.
- Regular Testing: Regular testing for chlamydia is important, especially for sexually active individuals and those who have new or multiple sexual partners. Early detection can lead to timely treatment and reduce the risk of further transmission.
- Partner Notification and Testing: If someone tests positive for this sexually transmitted disease, it’s essential to notify their sexual partners so that they can also get tested and, if necessary, receive treatment. This helps prevent further spread of the infection.
- Education and Awareness: Raising awareness about this sexually transmitted disease and other STIs is essential to help people understand the risks and take preventive measures. Educational campaigns can target schools, colleges, healthcare settings, and community organizations.
- Screening Programs: Implementing screening programs in high-risk populations, such as sexually active young adults, can help identify cases of this sexually transmitted disease early on and provide timely treatment.
Preventive and Regulatory Actions
- Healthcare Provider Training: Healthcare providers should receive training to properly diagnose and treat STD infections. They should also be well-informed about prevention strategies and the importance of counseling patients on safe sex practices.
- Vaccination (potential future measure): Research is ongoing for developing a STD vaccine, which, if successful, could be an effective tool in preventing new infections.
- Sexual Health Clinics: Establishing and promoting sexual health clinics like Phuket Medical Clinic that offer confidential testing and treatment for STIs, including chlamydia, can encourage individuals to seek care when needed.
- Contact Tracing: Contact tracing involves identifying and notifying individuals who may have been exposed to this sexually transmitted disease. This helps in breaking the chain of transmission and preventing further spread.
- Pre-Exposure Prophylaxis (PrEP): For individuals at high risk of STD, PrEP may be considered in certain cases. However, it is essential to remember that PrEP does not protect against other STIs, so safe sex practices should still be followed.

Prevention and control measures play a vital role in reducing Chlamydia outbreaks. By promoting safe sex practices, regular testing, partner notification, and education, we can minimize transmission risks. Implementing screening programs and training healthcare providers ensures early detection and proper treatment. Vaccination development could be a potential future aid. Contact tracing and sexual health clinics aid in curbing the spread. Emphasizing these measures enhances public awareness and responsible sexual behavior. Proactive efforts are crucial since this sexually transmitted disease can be asymptomatic. By focusing on prevention. We can effectively reduce the prevalence of STD, protect individuals’ health, and alleviate the burden on healthcare systems. Collective action is essential to safeguarding overall community well-being.
Complications of Hepatitis B
Hepatitis B is a viral infection that primarily affects the liver. It is caused by the hepatitis B virus (HBV) and is transmitted through contact with infected blood or bodily fluids. The virus can be contracted through unprotected sex, sharing contaminated needles, or from an infected mother to her baby during childbirth. Hepatitis B can lead to acute or chronic liver disease, with symptoms ranging from mild to severe. Acute hepatitis B infection may cause flu-like symptoms, jaundice, and fatigue, while chronic infection can result in long-term liver damage, cirrhosis, and an increased risk of liver cancer. Vaccination is available to prevent hepatitis B, and antiviral medications can help manage chronic infections. Regular testing and early intervention are crucial for effective management of the disease.